UVEITIS
What is uveitis?
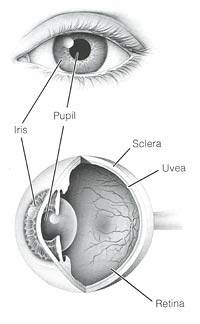
Uveitis is a general term for inflammation of the uvea, which is a tissue inside the eye. The uvea is made up of three parts:
- the iris (the colored part of the eye)
- the ciliary body (the muscles that adjust the lens and produce an eye fluid, the aqueous humor)
- the choroid (the layer of tissue just under the retina at the back of the eye).
How does it occur?
Most of the time, the cause is unknown. It can be related to certain autoimmune diseases that affect other parts of the body, like sarcoidosis and certain types of arthritis. Less frequently, infections like herpes, syphilis, or Lyme disease can cause uveitis.
What are the symptoms?
Uveitis that involves only the front part of the eye typically has the following symptoms:
- sensitivity to light
- redness
- tearing
- deep aching pain
- reduced vision.
These symptoms may occur in one eye only. They tend to appear suddenly and worsen quickly. When the middle or back portion of the eye is affected, the only symptom may be problems with your vision. You may see floaters (specks in your field of vision that look like little bugs or threads). Both eyes may be affected, but not to the same degree.
How is it diagnosed?
Your eye doctor will examine your eyes and ask about your symptoms. Usually he or she will dilate (enlarge) your pupils to help in examining the inside of your eye. Your eye doctor will look closely to see which parts of your eye are inflamed. Additional blood tests or x-rays may be necessary to make sure that there are no related diseases.
How is it treated?
Treatment is aimed at reducing the inflammation in your eye and making you more comfortable. Reducing the inflammation reduces the risk of complications later. Corticosteroid medicines are used to reduce inflammation. You may start using these medicines as eyedrops. If the eyedrops are not effective, your doctor may prescribe pills to take by mouth or shots around or into the eye. Corticosteroids may cause cataracts or high eye pressure. Your doctor will want to check your progress closely, especially if you use these medicines for a long time. Uveitis itself can also cause cataracts and high eye pressure.
If the inflammation is so severe that you need to take high doses of steroids or if the steroids are not helping, you may need to take another type of medicine called an immunosuppressant. These are related to chemotherapy drugs and you will need to be closely watched for side effects.
As the inflammation is brought under control, your doctor will give you instructions about how to gradually stop using the drops and pills. It is very important to follow these instructions closely. A sudden decrease in these medicines can cause the inflammation to come back. In those cases where the inflammation is caused by an infection, specific medicines to treat the infection are used in addition to medicines to control the inflammation.
How long will the effects last?
Like symptoms and treatment, the effects of uveitis depend on its cause. When the cause can be found and treated, you may not have any long-term effects. When uveitis is related to a problem that affects other parts of your body, the effects will last until you get proper treatment for that problem. Uveitis may come back. See your eye doctor promptly if any of your symptoms return.
If left untreated, uveitis can cause complications such as:
- high pressure inside the eye and permanent damage to the optic nerve
- cataracts (clouding of the lens of the eye)
- clouding of the cornea
- abnormal blood vessels inside the eye.
This content is reviewed periodically and is subject to change as new health information becomes available. The information is intended to inform and educate and is not a replacement for medical evaluation, advice, diagnosis or treatment by a healthcare professional.