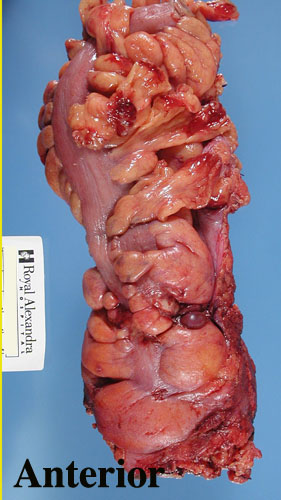

This is Philip Quirke's method for assessing colorectal adenocarcinoma as demonstrated for the MRC-CR07 trial participants. The first step is to assess the colon for completeness of mesorectal excision. A grade of 1, 2 or 3 (3 is best) is given. This particular example is a grade 3 completeness of mesorectal excision. Pay careful attention to the anterior mesorectum. This is where surgeons are more likely to cut into the mesorectum. A detailed account of the grading system is given on another page.
The mesorectal fat is inked and then the colon is opened above and below the tumour anteriorly but not through it. This best preserves the relationship of the tumour to the circumferential (radial margin). I probably opened a bit too much anteriorly in this case. Note how high the ink goes posteriorly, a reflection of the upper limit of the posterior mesorectum. I have been placing gauze in the lumen to wick the formalin into the lumen to allow better fixation. The main problem with this technique is the inability to observe the lumenal aspect of the tumour. In reality there is little to be gained from this observation with respect to margin involvement or anything else that might alter prognosis or management.
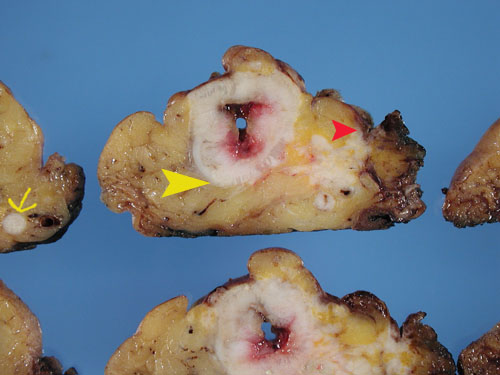
The colon is pinned and fixed for a minimum of 48-72 hours. This allows the tissues to harden sufficiently to allow very thin (3 mm) slicing of the tumour and of the tissues immediately above and below the tumour. The yellow arrowhead (below) highlights the smooth non-ragged contour of a proper mesorectal excision and also points to the tumour. The tumour is not well seen in this case since the patient is post radiotherapy. A minimum of 4 sections of tumour should be taken as well as sections of the circumferential margin and peritoneum if close by. We see exposed muscularis propria distally but this is acceptable since this is an AP resection and we are looking at exposed levators which are well below the mesorectum.
Lymph Nodes
I am extremely impressed by my increased lymph node yield
using this technique. The nodes stand out well and nodes as small
as 2 mm can be easily identified. Lymph node recognition is visual.
There are no clearing or opacifying agents used. I have been able
to reach the minimum number of 12 nodes recommended by the CAP.
Let it run
It is permissible to let margin ink run into any crevices
or mesorectal defects created by the surgeons blade. Ragged
mesorectal excisions are at increased risk for local recurrence due to
the likelihood of tumour spillage from lymphatics. Deep cuts into
mesorectum are therefore significant and are not ignored when the margin
is measured. The margin is deemed positive if tumour or mesenteric
deposits involve an erroneous surgical cut into mesorectum, even if the
mesorectal plane is distant.

Circumferential margin assessment
The measurement taken for the circumferential margin
is measured from tumour to circumferential margin or from lymph node or
mesenteric tumour deposit to the circumferential margin, whichever is closer.
The image (taken from another case) below shows the posterior limit of
the tumour (yellow arrowhead) while the yellow arrow and red arrowhead
show tumour deposits that are closer. The actual margin in this case
should be measured from the red arrowhead. The main tumour is close
anteriorly but it is lined by serosa at this point and thus does not count
as a margin. A positive margin is considered to be tumour within
0-1 mm of the circumferential margin.
This image should impress you more than anything else about how important it is to remove all the mesorectum so that tumour deposits such as this are not left behind.