Our local cancer institute has asked that gross pathologic
assessment of completeness of mesorectal excision (ie complete excision
of the rectal mesentery or mesorectal fat pad) be reported on all rectal
cancers. The purpose of this is to identify those patients who are
more likely to recur postop. giving prognostic information and thus
affecting followup and also to allow data entry into the cancer board data
bank for future study. This assessment will also be done for an upcoming
MRC trial (MRC-CR07). There is no doubt that complete mesorectal
excision will reduce local recurrence
rates (from 30-40% without TME, down to 3.7% with
TME (as reported by Heald)). Heald initially reported these findings
back in the mid-80's (Lancet. 1(8496):1479-82, 1986 Jun 28).
It is unclear why it has taken so long for this to catch on. Perhaps
it is because he does not practise at a major teaching institution.
John MacFarlane at UBC in Vancouver, frustated with high local recurrence
rates, went on sabbatical to Basingstoke, England to learn from Heald and
reviewed prospective followup data of Heald's work (Lancet. 341(8843):457-60,
1993 Feb 20) His paper stimulated a great deal of renewed interest
in Heald's surgical technique. In MacFarlane's words......
"Meticulous TME, which encompasses the whole field
of tumour spread, can improve cure rates and reduce the variability of
outcomes betweensurgeons. Far more genuine "cures" of rectal cancer are
possible by surgery alone than have generally been believed or are currently
accepted. Better surgical results are an essential background for the more
selective use of adjuvant therapy in the future."
Why can't the oncologists obtain their information
from the surgical report? Well apparently not all reported TME's
are actually total. Adequacy of TME varies from surgeon to surgeon.
This may reflect experience, training and ultimately the technique of the
surgeon involved. Dissection must be done with cautery or scissors.
No blunt dissection with the hand is allowed. Thus the oncologists
are asking for an independent second unbiased opinion. Only the pathologist
can do this. In addition, feedback from the pathologist will help
the surgeon improve his resections. Philip Quirke, a pathologist
from Leeds University is heading the pathologic aspects of the MRC-CR07
trial and has done more than anyone else to raise awareness of the importance
the circumferential resection margin and now assessment of TME.
A recent Dutch study (Nagtegaal et al. J Clin Onc
20: 1729-1734 2002) showed that pathologist assessment of TME predicted
a 36.1% risk for local and distant recurrence in patients with a grade
1 TME compared with 20.3% recurrence in grade 3 TME's.
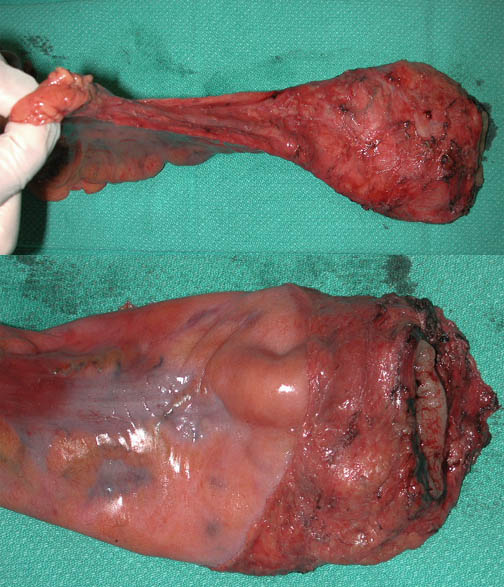
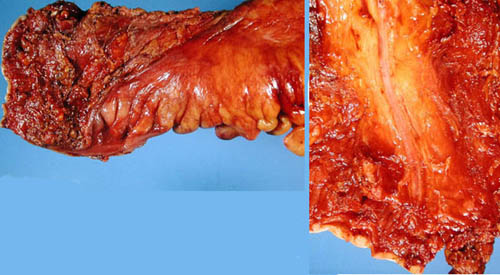
Cases 1 and 2 are examples below of what are felt to be total mesorectal excision by 2 different colorectal surgeons. The first one with the green cloth background shows a very smooth mesorectal fat pad. The fat pad also tapers distally consistent with complete excision of the mesorectum. This example was given to me by the colorectal surgeon himself. I don't think you can see a better depiction of a total mesorectal excision than this. I think this should be a grade 3 according to Quirke (see bottom of page). The second case (blue background) shows dissection of a mesorectal vessel contained within the mesorectum. The second case looks a bit ragged. This should be a grade 2 resection, not in agreement with the surgeon. The third case is another grade 3 and shows the wisps of fascia that surround the mesorectum indicating that a fascial plane actually does exist and also indicates that the surgeon has done a complete excision.
CASE 1. Total mesorectal excision. Grade 3.
CASE 2. Mesorectal excision. Grade 2.
CASE 3. Mesorectal excision, AP resection, posterior aspect. Grade 3. Note the fine wisps of fascia on the surface of the mesorectum
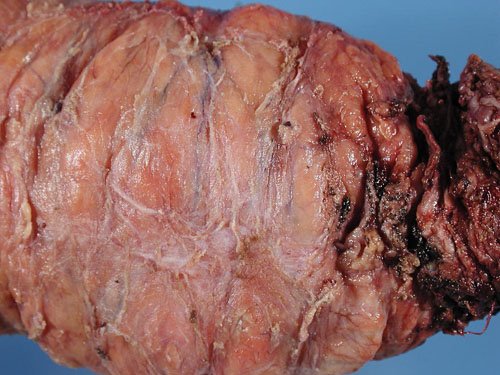
The next case shows a good smooth mesorectal fat pad but we see that not very much colon has been excised distal to the anterior peritoneal reflection (shown by the small margin of ink at the bottom end of the picture in the middle) thus the mesorectum has been completely excised to the distal margin but not removed in its entirety. As long as the mesorectum has been completely excised up to the distal resection margin this should be considered a grade 3 resection.
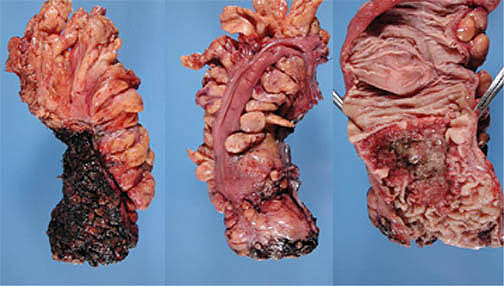
CASE 4. Complete mesorectal excision to the distal line of resection. Althoughentire mesorectum not removed (distal margin of resection is only just below the anterior peritoneal reflection - middle image) it is still consistent with a grade 3 mesorectal excision.
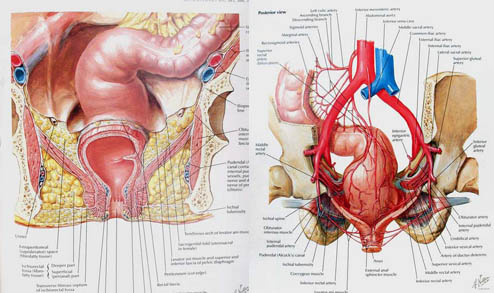
Pertinent anatomy is shown below (taken from Netter). Note the termination of the mesosigmoid (the proximal limit of the rectum) well above the peritoneal reflection in the drawing on the left.
Quirke's graded assessment of completeness of mesorectal
excision (MRC trial)
3-Good: Intact mesorectum with only minor irregularities
of a smooth
mesorectal surface. No defect is deeper then
5 mm. No coning on the
specimen. Smooth CRM on slicing.
2-Moderate: moderate bulk to the mesorectum but irregularity
of the
mesorectal suface. Moderate coning of the specimen
towards the distal
margin. At no site is the m.propria visible
with the exception of the
insertion of levator muscles. Moderate irregularity
of CRM.
1-Poor: Little bulk to mesorectum with defects down
onto m.propria and/or
very irregular cirumferential resection margin.
Notes
- Coning refers to the tendency for the surgeon to
cut towards the colon and breach the mesorectal envelope as he goes distal
rather than staying outside the mesorectal plane. This gives a tapered
conical appearance rather than a bulky distal mesorectal fat pad.
This can also lend a ragged appearance to the specimen since the surgeon
may realize his mistake and go outside the mesorectum to find the correct
plane once again, leaving gashes in what should be a smooth mesorectal
surface.
- Is it possible for the entire mesorectum to be removed
even though it has a ragged appearance? Yes, but it doesn't matter.
Once the mesorectum has been violated the risk for spillage of tumour from
lymphatics exists. A ragged specimen without a smooth surface must
therefore be a grade 2.
Links to
Method of dissection for colorectal
adenocarcinoma
Additional examples of TME
grading