Diabetes researchers at the University of Alberta and Cornell University have successfully combined two innovative surgical techniques for transplanting insulin-producing cells, offering people living with diabetes hope that the life-saving treatment could one day be made safer and more widely available.
In a paper published today in the journal Nature Biomedical Engineering, the scientists report sustained cell survival and diabetes reversal in mice that received subcutaneous islet transplants from other mice, rats and humans without using harmful anti-rejection drugs.
“If we’re to move our transplant therapy forward to treat children, or to treat patients who have very stable, easy-to-control diabetes or Type 2 diabetes, we need something that’s going to cause less harm,” says James Shapiro, Canada Research Chair in Transplant Surgery and Regenerative Medicine and professor of medicine and surgical oncology at the U of A.
“If we could do a transplant with less or no anti-rejection drugs, we could do it much more safely, and we could include more patients who could benefit.”
Shapiro cautions that while the results seem promising, the method needs to be further tested in larger animals, and eventually in humans, to know its full potential.
Shapiro leads the Edmonton Protocol, which has allowed 750 transplantations of donated islet cells since it was first developed 21 years ago. Many of those patients no longer need to take insulin injections for their diabetes but they face a lifelong regime of anti-rejection drugs, which can make patients vulnerable to infection and even cancer.
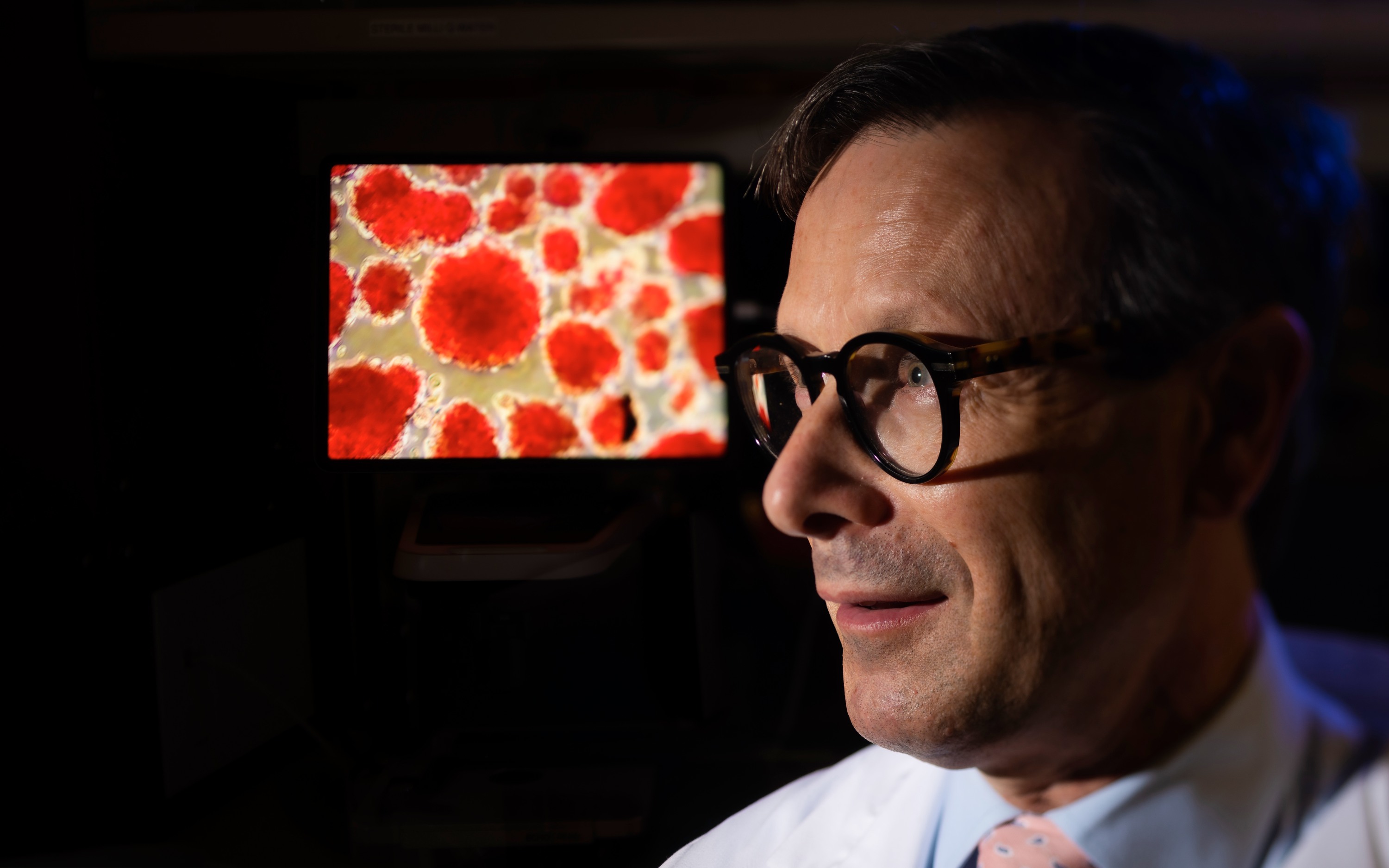
Shapiro has devoted his career to perfecting the transplantation technique and making it more accessible. Though most successful islet cell transplants are currently grafted into the liver, it is not considered an ideal site because it’s hard to monitor or remove the transplanted cells from the internal organ. In 2015, Shapiro’s team created a potential alternative transplant site under the skin by placing a plastic tube in the forearm, allowing blood vessels to form around it, then removing the device, leaving behind a vascularized pocket for transplantation.
In 2017, Shapiro read about another transplantation innovation from Minglin Ma, professor of biological and environmental engineering at Cornell University, and invited him to collaborate. Ma and his team had created a removable polymer thread containing thousands of islet cells protected by a thin hydrogel coating that could be implanted into a patient’s abdomen without triggering an immune response.
“I was intrigued by the virtue of Ma’s approach as it avoided the need for immunosuppression, and I wondered if we might combine our two innovative strategies to improve cell survival,” recalls Shapiro. “And indeed it worked! By combining the two, it really did improve the skin site for engrafting cells without the need for anti-rejection drugs. The data are very compelling.”
The teams have named their new combined approach “SHEATH,” which stands for subcutaneous host-enabled alginate thread.
“It was a great idea by Dr. Shapiro to build on two separate, very strong approaches for islet transplantation,” says Braulio Marfil-Garza, who won the Governor General’s Gold Medal for his PhD research in Shapiro’s lab and is now director of pancreatic islet transplantation at Tecnológico de Monterrey. “This was the perfect synergy.”
“We are really serious about pushing this into something clinically applicable, something that’s impactful,” says Ma, whose student Long-Hai Wang, now a professor at the University of Technology and Science of China, worked with Marfil-Garza to conduct the experiments.
Marfil-Garza believes the method should also be tested for transplants of other types of hormone-producing cells for diseases such as anemia and chronic renal disease. He is establishing a brand new islet transplant program in Mexico, with plans to treat the first patient in February 2025.
Shapiro, who is a member of the Alberta Diabetes Institute, is collaborating with Ma to seek funding for more research on the SHEATH model. He also continues to search for a new source of islet cells for transplant by growing them from stem cells.
“We want to have multiple shots on goal, so we work on multiple projects in parallel,” he says. “Nine ideas out of 10 in the lab typically will fail and it’s only the one out of 10 that moves us forward to the next step. That’s just the reality of doing scientific research.”
The research was supported by the National Institutes of Health, Novo Nordisk, the Juvenile Diabetes Research Foundation, The Hartwell Foundation, the Diabetes Research Institute Foundation of Canada and others.