
Discovery
Discover the truths and stories behind monosodium glutamate

Discovery
Brew, Beauty and Bounty: A curated list of U of A-linked grad-owned, Canadian-based small shops

Commentary
Your questions about the topsy-turvy U.S. trade war answered

Feature
Water shapes life here on solid ground. But our effect on life underwater is as substantial as our need to better understand it

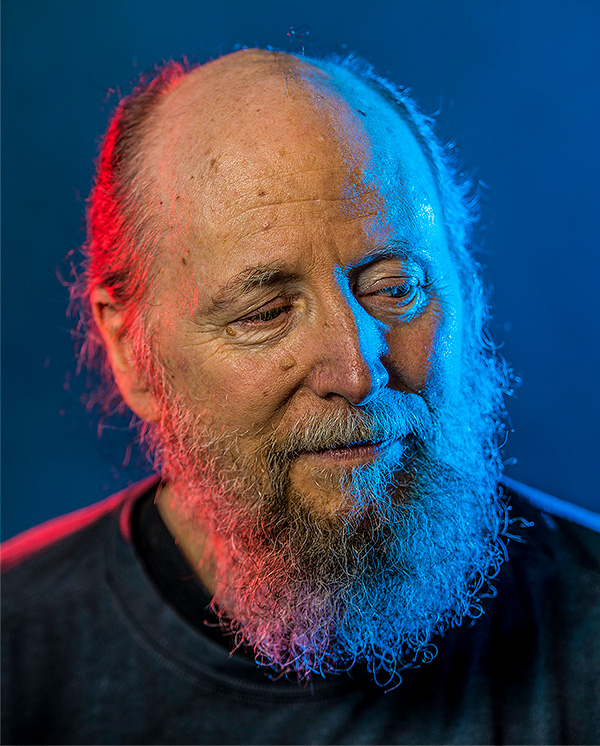
2024 Distinguished Alumni Award
Atul Malhotra is driven by passion, opportunity and necessity — but mostly the people in his community

Discovery
The first-ever meteorite to land in P.E.I. is caught on camera and makes auditory history — now it’s at the U of A

Society
Level up your civic engagement

Feature
Neither individual actions nor general goodwill can protect and restore the land we rely on. But expanding our perspectives and adopting systems thinking just might.

Profile
One grad knows that good policy can change the way we incorporate AI into our systems and lives

Tech
Generative AI can promote or inhibit students’ learning, which poses a challenge for educators and parents

At Home
Five books that will transport you around the world

Profile
By giving Indigenous students space, Indigenous cultures regain their place

Research, Health and Wellness
A community health nurse looks to an Elder for help talking about tough mental health subjects

U of A in Your Life
Tools like ChatGPT have their uses but make sure you know the limitations

Just for Fun
Paulette Breault shares how a memorable ride launched her 50-year love story

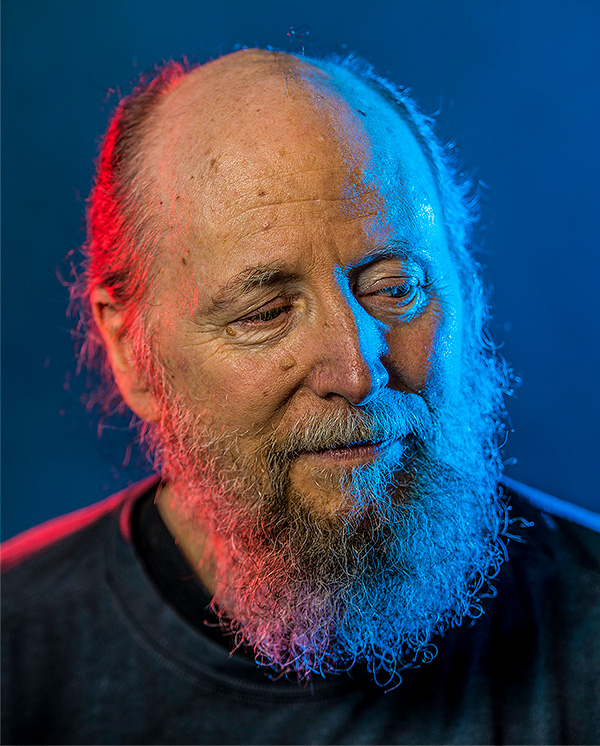
2023 Distinguished Alumni Award
Bob Bertram’s methods have changed the way pension funds operate around the world

Society
Being a non-verbal communicator requires some technology, patience, humour and a whole lot of persistence

Continuing Education
They say it’s the journey that matters. But when that ‘journey’ includes furniture repair with limited skills, it helps to have an empty basement and an open mind.

Society
Justin Tetrault, a criminology professor at Augustana Campus, recently gave a talk about his research. Here are a few takeaways

At Work
Classrooms are a bit like students in that each has a unique personality and no two are alike

Did You Know
When we power down for the night, our brains light up, creating and storing long-term memories

Did You Know
This traditional art is Tara Kappo’s ‘medicine,’ linking her to her relations, human and non-human.

Tiny
Researchers are harnessing everything from tiny tech to microscopic cells to treat major health threats

Thesis
Swapping lectures for in-class activities is flipping the script in law classrooms

Research
Scientists are harnessing quantum mechanics to create computing power beyond anything we’ve ever known

Profile
Advice from a Giller Prize-winning author

Continuing Education
Seems like just yesterday I lightened my parents’ load by moving out. Back then, I couldn’t imagine why it was such a big deal

Health
The microbes in your digestive tract can affect everything from your immune system to behaviour

Distinguished Alumni Award
Well known for Corner Gas, Lorne Cardinal’s career has made him an Indigenous role model and advocate

Just for Fun
Step away from the Mr. Noodle

Feature
Today’s challenges and how we address them will shape the way we live

Health
No matter what you do, having a support network can get you through, says U of A researcher

Health
Many people could benefit from getting more plant- and animal-based sources in their meals

Living
A former U of A sociology professor refused to accept Japanese internment. Now his story is on the stage

Living
What we say when we avoid talking about death

Distinguished Alumni Awards
Meet the 2021 Distinguished Alumni Award recipients, who are helping to preserve land and life

At Work
A business grad-turned-poet shares tips to turn your passion into a day job

Thesis
From lapdogs to sentries, our canines are part of many cultures in a way no other creature is

Health
Many affected women are embarrassed about their common urinary condition. But help is here

Profile
You don't have to be at the top to lead, say former U of A and UBC presidents

Environment
Used right, fire is a tool for renewal and connection with the land

At Work
Before you give up on an underperforming employee, find out how you can turn things around

Just for Fun
One of my favourite profs assigned a seminal Dostoevsky novel 30 years ago. Would I ever finish it?

Health
Life is supposed to get back to normal. So why does it feel like we’re entering the unknown?

Walking Together
The land and all its beings are central to Indigenous beliefs

Environment
For this industry, sustainability is more than a buzzword. And it’s coming to our farms and dinner plates

Just For Fun
Cooking together is as much about telling stories as it is about recipes

Society
Wish your neighbourhood was more walkable? Have some feelings about the bus stop in front of your house? Become a part of the solution with these tips.

Walking Together
Indigenous Peoples agreed to share the land — with conditions. It’s important that we learn and talk about what that means

Just For Fun
You might learn something about romance

Continuing Education
Free online course offers advice to help you separate fact from fiction

Continuing Education
One grad shares what crisis taught her about rolling with the punches

Health
Menopause gets the research treatment

Alumni Awards
This Earth scientist is one of four 2020 Distinguished Alumni Award recipients

New Trail 100
During the First and Second World Wars, the magazine connected grads serving overseas to those a little closer to home. The archives offer a glimpse into those times

New Trail 100
A trailblazing mountaineer. A well-loved governor general. The magazine’s first decade featured some fascinating characters

New Trail 100
We dug through the New Trail archives and found articles that showed just how well grads and researchers could predict the next big thing

At Work
Because pandemic or not, those one-shot first impressions aren’t going anywhere

Thesis
If you can’t travel widely, travel deeply

Society
Dig into this contentious call to action

Continuing Education
What my friend asked of me took some heavy lifting and a fundamental shift in my thinking

Feature
When COVID‑19 hit, the U of A, home to one of the world’s pre-eminent virology institutes, was ready

Living
This probably isn't what you had in mind

At Work
When your job involves keeping front-line workers safe, you never get a day off

At Work
Learning how to teach in the age of physical distancing

At Work
From attending a birth to running a bingo: a recreation therapist's surprising roles

Relationships
How to pandemic-proof your relationship

Health
Experts offer creative tips to keep loneliness at bay

Did You Know
An average dude pays attention to his wife's classical music. And he has some feelings about it

Thesis
We change our minds all the time. What makes our decisions easy or hard?

Continuing Education
I took 'be prepared' to a whole new level on my summer hiking trip. I like to think that's why I'm still alive

Just For Fun
A sleuth uncovers how a UAlberta prof's quote was credited to a U.S. judge - and why it matters

Feature
This year's Alumni Award recipients have made change around the world

Living
Discover the secret stories of stuff in this surprising U of A collection

Continuing Education
In life, as in baseball, we often dream of a home run rather than keeping our eye on the ball every time at bat

Did You Know
Tradition is central to health in the Northwest Territories

Living
Strategies to foster inclusion and help you broaden your community

At Home
'We have everything we need and nothing more, and somehow that makes everything simpler'

Tech
There's no such thing as a free orbit

Energy
By reducing the friction in pipelines, a researcher looks to make them safer and more cost-effective

Energy
We asked some alumni working in the energy sector to tell us what they see as the biggest challenges in the next five to 10 years. Here's what they had to say.

Energy
Grad students are adapting centuries-old engine designs to capitalize on abundant geothermal energy

Energy
Methane-eating bacteria already exist, so why not put them to work for us?

Money
Don't give away the money that could stay in your pocket

Health
Jump into the Bod Pod to find out what you're made of

Environment
Don't be fooled by their cuteness. Coyotes, Canada geese and raccoons are just waiting to take advantage of you

Living
Remove the throw rug, add a smartphone and more tips to keep your parents safe

Relationships
Conflict won't solve itself. But a good talk can clear the air - and the misunderstandings

DIY
Don't let the name put you off. Infusing alcohol with botanicals is easy and delicious

Living
Don't just worry about the money you'll spend. How will you spend your time?

Continuing Education
Sometimes acting your age is more fun than you expect

Living
Don't settle for pinchy or floppy footwear. You're better than that!

Business

Relationships
Find out what you can do when something seems wrong

Thesis
However we slice it (or bake it), bread is so much more than something we eat
Alumni Awards
Rob Daum, '82 BPE, '84 BEd, hockey coach

Continuing Education
My wife's extended holiday at home has rattled my routine and taxed my, er, productivity

Living
10 ways to make the time together more meaningful

Health
Countries and communities are taking action to change attitudes and keep people safe

Money
We get so busy with our day-to-day lives, it's hard to plan for the future. But it's coming

Thesis
Science is uncovering what's behind the canine-human bond

Continuing Education
From The Gateway to Guardians of the Galaxy: How one of the top artists in comics worked his way into the business
Profile
No. 1: artificial intelligence isn't really artificial

Did You Know
Forget everything you've learned in the movies. AI is so much less - and more

Tech
Prosthetics learn to predict a person's motions to operate more naturally
Tech
Artificial intelligence is here to stay. We look behind the hype

Money
The lessons I learned on the road to buying a condo

Did You Know
We forget almost everything, so what sticks and why?

Did You Know
Our social circles are overlapping more than ever

Tech
7 ways to avoid the aches and pains of texting

Profile
A helping of humour (+ a pinch of profanity) keep this cooking series bubbling.

Just for fun
How my family's campus roots added meaning to my education
Continuing Education
Being forced by an injury to take it slow offers valuable lessons on life — though I'd rather have been golfing
Living
There is value in contemplating the impact of our education and the places that make it possible
Alumni Awards
Teresa Spinelli, '83 BA, Businesswoman
Alumni Awards
Heike Juergens, '72 BA, '79 MEd, '87 PhD, psychologist, volunteer extraordinaire
Alumni Awards
Gail Powley, '84 BSc(ChemEng), engineer

Profile
Association president-elect looks to harness the time and talent of alumni

Feature
Métis author unpacks pervasive misconceptions

Feature
A teacher explains how his world travels in search of classroom inspiration turned adventure into activism

Feature
Education is essential on the path to reconciliation, the TRC emphasizes. But implementing the wide-ranging calls to action is a slow and complex process, as many at the University of Alberta are beginning to realize.
Feature
Three artists reflect on their work related to truth and reconciliation

News
U of A alumni who made headlines recently

Health
Study finds daily text messages help manage anxiety and depression

Discovery
A new type of electrical system could soon make power lines obsolete
Commentary
An elder talks about what the treaties mean to Indigenous peoples and what it means to teach and learn in a traditional way

Just For Fun
Newest MOOC highlights essential role of world's peaks

At Work
My most embarrassing jobs (go-go dancer?) taught me the most

Environment
Over the last two million years, most of Canada has been covered and uncovered by glaciers. Now these glacial ice cores reside in a state-of-the-art lab at the U of A
News
A brief look at what's new at the U

News
A brief look at what's new at the U

Profile
Just For Fun
Answering the question: What if our biggest discoveries were made into movies?

Health
A U of A team is looking to unleash the immune system so that it attacks powerful cancer cells and heals itself

Society
Claire Edwards may be the most civic-minded young woman ever, and is an expert on getting young people involved in their communities.
Did You Know
From the Collections
Discovery
Catch up on the lastest news about the U of A and alumni

Discovery
Fifty-five composers turn sounds captured from Earth's magnetosphere into music

Discovery
Physicist Don Page talks us through the science behind Stephen Hawking's recent headline-prompting pronouncement

Money
New platform gives students and researchers a new way to raise funds

Feature

Profile
Laila Steen is the first to admit that having an arts student pursue a science degree seems pretty weird

Did You Know
A partnership between the U of A and the father of India's 'Green Revolution' is yielding results for thousands of Indian families

Society
Alumni Pride chapter and a $5M campaign mark a new era

Living
Drama prof David Ley is the man of many voices

Did You Know
Construction begins on the new Physical Activity and Wellness Centre

Environment
What you'll find at the U of A's Circumpolar Library

Discovery
U of A researchers help find the elusive Higgs Boson

News
New Saville Community Sports Centre unites the community through sport

Just For Fun
U of A students, faculty and alumni gear up for another record-breaking challenge

Just For Fun
You're invited to share your U of A library stories in celebration of Rutherford's milestone.

Profile
An alumnus leaves his alma mater's mark at the North Pole during a once-in-a-lifetime trip.

Notes
Augustana forges an exciting partnership with liberal arts college in China.

Tech
One-of-a-kind machine allows researchers to expose the past of samples by analyzing their atomic makeup.

Discovery
Research expert Andre Martel shares his fascination with the tastiest of bivalves...mussels.

Feature
Four Panda's Hockey alumnae look back at their championship season.

Health
ELLA-Edmonton Lifelong Learners Association promotes well-being for adults 50-plus.

Tech
A design grad's 3-D simulations get super-sized

Tech
U of A Professor Marc Mackenzie dubs a tweet by Stephen Fry "the most beautiful Twitter message ever composed"

Profile
Cathy Allen brings her green and gold pride — and quilting skills — to the U of A community

Alumni Recommend
U of A grads take over your bedside table

Living
Two former Pandas wrestlers reflect on participating in Canada’s biggest race

Health
Building different takes persistence

2024 Distinguished Alumni Award
Linda Ogilvie worked across differences to improve the field of nursing around the globe

Profile
Grad bridges biotech innovation and community service, helping transform his adopted city into a research powerhouse

Continuing Education
I met the limitations of my judgment when navigating the space between conviction and flexibility

Thesis
There’s no magic bullet to managing my migraine, but learning a little about myself has helped

Alumni Impact 2024
Don’t wait in the shadows. Take chances and don’t underestimate your own abilities.

Trails
One grad’s path to veterinary medicine

Alumni Impact 2024
At the writing camps she runs, Gail Šobat sees how creative outlets can help kids navigate a complex world

Living
A sports mental trainer gives tips for healthy competition

Did You Know
Death is scary, but getting your affairs in order doesn’t have to be

Feature
Tools like ChatGPT are already having an impact on our learning, our jobs — even on our sense of what’s real. Experts weigh on what to expect.

Health
Expert offers insight into the role of physical therapy in cancer patients’ mental and physical recovery

2023 Distinguished Alumni Award
As a doctor, professor, researcher and mentor, Bruce Ritchie works doggedly for the best treatment for patients

Thesis
The revolution is incremental

At Work
Experts bust some myths about starting a business

Living
A visual artist and fine arts instructor shares his four-step method

Just for Fun
John Acorn, a.k.a. the Nature Nut, shares tips to embrace the great outdoors this summer

Did You Know
From bees to bats, pollinators are key to a stable food supply

Profile
Telling the stories of the grads who came before deepens our connection to the U of A and to each other

Did You Know
One of the world’s most widely spoken languages offers a passport to Chinese culture

Environment
Researchers are targeting threats to our climate and food supply — some of the answers are smaller than you think

Tiny
The U of A is full of tiny marvels – from miniature items to microscopic research

Relationships
How to tend to the care and feeding of romantic bonds

Tiny
Ice that’s tens of thousands of years old helps us study the past and peer into the future

Distinguished Alumni Award
Brian Haynes created a service that puts the best of health research at doctors’ fingertips

Continuing Education
A taste for the red stuff has created surprising similarities across species — and across research interests

Feature
Communities around the globe are struggling to remain viable. How can we stop their decline?

Did You Know
What to do when you see wildlife on urban trails this summer

Thesis
Student clubs give participants a taste of what it means to work together on a complicated and multifaceted design project

Tech
Instead of a career in journalism, one arts graduate launched a startup to neutralize internet toxicity with technology

Feature
Can sunshine be improved? Can paralysis be reversed? Four researchers push the bounds of knowledge to change lives

At Work
Edmonton business demonstrates that supporting startups is limited only by imagination

Health
Medicines or treatments that work for one patient or group might be less effective for another

Continuing Education
Unlock the innovator within you with these steps

Thesis
What happens when the idea of “us” grows, allowing it to encompass a little more than it did before?

Continuing Education
These aren't your average inspirational quotes

At Work
It’s creative, fulfilling and it might just change your life

Profile
Life lessons from a teacher, skateboarder and team player

Just For Fun
If you love lifelong learning, and love (or loathe) insects, read on

Society
No two treaty agreements are alike, but all of them offer a lot to the people who reside on treaty territory

Health
How to inspire kids to get (and keep!) moving on their physical literacy journey

Thesis
What mentors have to learn from their mentees

Society
COVID-19 changed how we process, ship and shop for food. What supply chain changes will stay into the future?

Did You Know
Meet your new alumni president

DIY
Five tips for using and improving the online encyclopedia

Society
It’s going to be messy, difficult and emotional — and worth it

Technology
Could this 12-year-old technology put the ownership of our personal data back in our hands?

Health
How a pandemic and an international movement for civil rights converged to throw light on flawed systems

Society
There’s no shortage of stories to help you shift your gaze and see things in a new way

Alumni Awards
The former president of Yukon University is one of four 2020 Distinguished Alumni Award recipients

Alumni Awards
This former deputy minister is one of four 2020 Distinguished Alumni Award recipients

News
The plan also prioritizes student experience, Bill Flanagan told alumni at a virtual town hall

Just For Fun
Take one down, pass it around, how many local breweries in all?

Society
In turbulent times, educators need amazing mentors

New Trail Classic
In this profile reprinted from April 1969, then-U of A president Walter H. Johns worries about the ‘desperately serious’ pessimism of ‘these long-haired types’ at the height of the counter-culture era

Walking Together
I dread to think of my young grandson suffering that pain. It’s up to all of us to continue the ‘heart work’ toward understanding

Discovery
U of A labs are part of the worldwide hunt for solutions

Feature
Instead of playing catch-up with the next new virus, precision medicine aims to let us find it early and deal with it swiftly

Living
Grad Andrew Parker talks about demonstrations and conversations in a time of change

Feature
Research shows talking about it can make us stronger. And that we can learn how to find it

At Home
How video games keep people connected

Living
It's good to review your estate planning, even in the best of times

Health
A psychiatrist's guide to busting up bad thought patterns

Living
Start small, with simple kindness

At Home
These aren't your typical staff picks. Here's a curated booklist to broaden your horizons while you're holed up at home

Living
Life lessons from a grad who dropped everything to sail halfway around the world

Thesis
Not everyone's brain operates the same way. Shouldn't we try to make the most of it?

DIY
These treats fuelled the studies of UAlberta students for decades

At Home
Here's a reading list that will fire up even the most reluctant readers

Feature
As chief justice of Canada's highest court, she helped define some of our most fundamental rights. What drives Beverley McLachlin?

Thesis
A registry of twins will let researchers look deeper into what factors influence our health and behaviour

Thesis
There's no way to level the playing field but we can aim to do better by each other more often

Health
It took me three tries to find the right counsellor. I'm glad I didn't give up

Thesis
Our ability to tinker is allowing us to travel farther than ever

Tech
An interdisciplinary centre allows you to virtually venture where you couldn't before

Energy
Social sciences and humanities help us examine the challenges of energy systems

Energy
Researchers look at ways to make our energy projects more people-friendly

Energy
When you hit the switch, the lights have to come on. Read about the challenge of powering the next generation

Energy
Our myriad devices, vehicles and appliances require more energy all the time. These research breakthroughs are poised to lessen the rate at which we burn energy, improving how we generate and store power.

Did You Know
The new Alumni Association president begins her two-year term in June. We caught up with Heather Raymond, '82 BEd, '86 Dip(Ed), '95 MEd, '02 PhD, a retired teacher and principal, to find out what keeps her energized as a volunteer.

DIY
Assembly definitely required, but here's the instruction manual

Just For Fun
UAlberta grads on why they couldn't get enough of the Tuck Shop cinnamon buns

Health
At least they're your germs. Imagine what's crawling on the plastic bins at airport security

Money
Get weird. Be selective. Don't wait.

DIY
Try making your own ink. It lasts much longer than that disposable pen in your pocket

DIY
An artist breaks down her favourite painting into 6 simple steps for even the most artistically challenged.

Did You Know
Stretch your vowels - and your confidence - with these tips on talking to a crowd

Tech
(Find out what separates it from a dumb machine)

Living
Know what you want from a tree and learn how to make it last through the holidays

Health
Plus U of A experts field questions about cannabis

Thesis
Your city in tough times: true hunger is never far away

Thesis
Have we seen the future of meat?

Alumni Awards
Fear and misconceptions in the early days of HIV

Trails
Author Jason Lee Norman, '06 BA, transforms a campus memory into a work of flash fiction

Feature
Reimagining the way we care for people

Health
Hopes for an Alzheimer's treatment are raised, then dashed, but can we tilt the odds?

Thesis
It comes down to something called the friendship paradox

Thesis
One scientist's research on anesthetics might help find the answer

Living
Researcher tests fabric to rank the funk in the armpits of your T-shirts

Continuing Education
Life lessons from marathoner Natalie Shanahan, '06 BSc(Kinesiology), '09 MSc

Continuing Education
After five decades on the planet, I'm still searching for the balance between 'laid back' and 'lava'

Tech
Unexpected behaviour offers clues to how artificial beings learn
Unexpected behaviour offers clues to how artificial beings learn

At Work
Expert advice on navigating the job search without sacrificing mental health

Profile
Thing 1: He once gave a TEDx talk about gallstones

Did You Know
How resourceful Cubans get their Netflix

Continuing Education
4 tips to help uncover and overcome your unconscious biases

Tech
What parents need to know to keep kids safe

Just For Fun
Author transforms a campus memory into a work of flash fiction
Just For Fun
We asked alumni to share the most popular (or worst!) fashions while they were students

Discovery
Discover five groundbreaking objects that you might be surprised have a U of A connection and hear from experts about their national, global and sometimes very personal impact.
Alumni Awards
Margaret Evans, '14 BA, foreign correspondent, CBC

Profile
Lorne Warneke, '63 BSc(HonsCert), '67 MD, psychiatrist, clinical professor
Alumni Awards
Donald Brinton, '51 BSc(Ag), Broadcaster

Feature
After seven years spent listening to residential school survivors, two TRC commissioners remain hopeful about the future

Feature
Three students and one alumna talk about their university experiences

Feature
A romance author takes us beyond happily-ever-after

Feature
Here are just some of the many ways to begin educating yourself
News
A brief look at what's new at the U

Did You Know
The story behind the switch from newspaper to magazine

Living
Clothing opens door to outdoor activity for those with limited mobility

Discovery
U of A research is always garnering media attention. Here's the lowdown on what's been causing a buzz.

Continuing Education
A course in Swaziland offers MD student a new world perspective

Did You Know
International research team discovers two never-before-seen celestial phenomena

Environment
U of A community steps up during massive emergency evacuation of Fort McMurray area

News
U of A research is always garnering media attention. Here's the lowdown on what's been causing a buzz.

Discovery
Electrical engineering PhD students use ultrashort laser pulses to weld neurons together

Discovery
75-million-year-old baby dinosaur skeleton by U of A paleontologists hailed as one of the rarest finds to date.

News
U of A alumni who made headlines recently

Did You Know
Thomas Dang has gone from U of A lecture halls to a crash course in "how to be an MLA" as part of his new role as a member of the Alberta government

Health
For people living with a recurrent C. difficile infection, everyday mealtime becomes a painful test.
Discovery
U of A research is always garnering media attention. Here's the lowdown on what's been causing a buzz.

Environment
Ross Lockwood spent his summer vacation on Mars... or at least a simulation of Mars on the slopes of a volcano

Discovery
One U of A researcher argues that genes are followers, not leaders, when it comes to evolution

News
Former PM has been named founding principal of the Peter Lougheed Leadership College
Did You Know
Uncovering campus treasures

Profile
Being a leader is something Nisha Patel strives to embody every minute of the day

Environment
U of A weather expert Gerhard Reuter answers the question what is a Frankenstorm

Discovery
Curiosity-driven research on Arctic mosses turns up unexpected findings and makes Catherine La Farge a rock star in the botany world.

Profile
Megan Engel, '12 BSc, becomes the 69th U of A student to receive a Rhodes Scholarship
News
Stories from our campus community

Health
Alumnus competes in second Ironman triathlon 25 years after receiving heart transplant

Did You Know
U of A professor receives America's highest civilian award

The work of internationally recognized virologists at the University of Alberta has propelled the University to the front lines of a biological war against viral disease.

Environment
Canadian Mountain Studies Initiative brings together scholars attempting to understand mountains in a global context

Discovery
Discovery of new 'adaptin' protein may offer insight into the cause of some neurodegenerative disorders

Did You Know
Faculty of Medicine & Dentistry graduates first female neurosurgeon.

In Memoriam
The U of A Alumni Association pays tribute to alumnus and literary icon Robert Kroetch.

Health
New U of A Calgary speech institute helps adults and children overcome stuttering.

Discovery
U of A astronomer's research reveals the "weird" physics inside a neutron star

Feature
Writer and alumna Aritha van Herk on the rewards and risks of friendship

Feature
Take a peek inside the U of A's new one-of-a-kind CCIS building.

Continuing Education
Braden O'Neill, '09 BSc, is the University's 65th Rhodes Scholar

Did You Know
Third-year U of A student Paula Finlay has become the only woman to win back-to-back triathlons this WCS season.

Profile
Libe Garcia Zarranz is awarded $180,000 as one of this year's 15 Trudeau Foundation Scholarship winners.

Health
An addiction recovery physician busts myths surrounding the complex disease

Thesis
If possibility is endless, our experiences are the only things that are real

Feature
To solve the puzzle of sustainable sustenance, researchers boost crop yields, combat pests and create new foods

Living
What does it take to find joy in the concrete jungle?

2024 Distinguished Alumni Award
Robert Philp is committed to protecting human rights, advocating equality and advancing education

Profile
Your new director of alumni relations shares how to harness the power of community

Profile
Lessons from a man who tossed the family playbook and embraced a different path

Money
Neurodivergent, queer financial educator shares top tips to make your money work for you

Profile
Friendship builds a strong foundation for teamwork

Continuing Education
Growing up with five siblings made me competitive. Later, I discovered a dark side to competition

Alumni Impact 2024
Linda Ho and her team merge food science with the culinary arts to create tasty new local products

Alumni Impact 2024
An offhand idea sparked a husband-and-wife business that harnesses fruit flies to develop life-saving therapies

Did You Know
Fundamental quantum research could lead us to a whole new scientific reality — one with answers to the biggest problems of today and tomorrow

Discovery
From chatbots for seniors to efficient construction, U of A researchers are using artificial intelligence to enhance our lives

2023 Distinguished Alumni Award
“Every single person who lived through COVID lost something in some way,” says Deena Hinshaw, former Alberta chief medical officer of health

2023 Distinguished Alumni Award
As a plastic surgeon, Gordon Wilkes dedicated his career to helping people with missing features of the head or neck

Did You Know
Generative AI models may sound like us, but to truly understand language requires human experience

Just for Fun
Practice, place and pacing are key

Health
Gradual hearing loss can impact your well-being, but help is available

Health
Good vibes and good friends are a good start

Profile
Ashton Rudanec started her two-year term on June 1

Thesis
A former 4-H club kid has to ask, can people actually learn without doing? It turns out there is no solid line dividing the two.

Feature
Researchers are developing small molecule drugs to treat everything from age-old threats to modern menaces

Tiny
Enter the weird and wonderful world of quantum physics

How-to
U of A researcher offers tips based on successful reading intervention program

Tiny
When language ebbs and flows, students get creative

Health
Four reasons to stay active during cancer treatment

Distinguished Alumni Award
Robert Foster’s tenacity has his small pharmaceutical company punching above its weight

Profile
One grad is on a quest to revitalize Denesųłįné in her community

Thesis
Humans can’t help but create — the evidence is in our books, our gardens and even in our gods. And in enacting our creativity, we define our humanity

Continuing Education
I grill it, flip it and serve it, all to perfection. But my reasons for not eating it are less global change and more personal challenge

At Work
A psychologist offers tips to help you change your mind about yourself

Thesis
The edge is a zone of transformation and discovery, at once a marker between distinct areas and a place of its own

Society
There’s nothing I can do for my family in Ukraine except plan for better days
Society
Speech language pathologist helps trans patients find their best vocal registers

Society
How one grad’s journey through the past helped her better understand her present

Living
It’s winter. It’s supposed to be cold, and I’ve finally learned to like it

Discovery
Turns out having all-star scientists on board draws students, researchers and funding that boost the economy

Relationships
Two decades after we graduated, we’re learning about life from our Gateway friends all over again

Thesis
Sometimes a map shows the way to a place. Sometimes it points to a memory.

In Memoriam
I feel like I know you, but the attack on Flight PS752 has robbed us of the chance of real friendship

Living
Expert tips to help you find information you can trust

At Home
Spoiler alert: everyone’s going to be OK

Continuing Education
7 tips to build an interesting career (and life)

Environment
In the drive to become more efficient and adaptive, farms are becoming innovation incubators

Discovery
What does it take to win the world’s top prize in medicine? Inside Michael Houghton’s seven-year hunt for a mystery virus

Environment
The clothing industry needs to change, and we can help

Living
Prepare your pooch for post-pandemic life

New Trail 100
What does a grad from 1953 imagine he would find at the U of A in the 21st century? Giant Rabbits

New Trail 100
Researchers have been solving problems in our lives for 100 years — and they’re still at it

Health
The Nobel laureate talks about persistence, post-COVID-19 virology and when 'the thinking' happens

New Trail 100
Pranks have always been a staple of U of A life, but this one from 1926 left us with eyebrows permanently raised

Alumni Awards
This infectious diseases specialist is one of four 2020 Distinguished Alumni Award recipients

At Work
4 tips to overcome the dread and make important career connections

Thesis
Can’t follow that street map? It’s not you, it’s a design flaw

At Work
There’s no sales pitch required

Discovery
Innovators aren’t holding their breath for a vaccine — they’re tackling the biggest health crisis in a century on several fronts

Environment

Profile
Where most people see challenge, Bill Flanagan sees opportunity. He returns to Alberta to face his biggest challenge yet, as the U of A’s new president

Just For Fun
If there were a dating site for bugs, what would it look like?

Feature
Pandemics shape societies as much as they do public health practices, exposing rifts and new potential

Commentary
With the small amount of solace I can offer, I myself am comforted at heart

Money
The first-timer’s guide to a post-pandemic investment planning

Alumni Recommend
Here's a list of arty stuff to see, do, watch and try. It'll help you enjoy and understand the times we're in

At Work
COVID-19 is taking a toll on companies. Owners offer some helpful tips

At Work
Three instructors share their tips for teaching online

At Home
A home-schooling veteran offers ideas from her own experience

How-to
A psychologist's tips on how to guide young ones through times of uncertainty

In Memoriam
Friends remember Mohammad Mahdi Elyasi, '17 MSc, as kind, creative and motivated

Thesis
Learning is labour, and memory socks away its yields for a rainy day. But how we learn and recall involves surprising processes - and body parts

Feature
Former students remember these treats with a passion. We investigate their mythical status

Did You Know
A bench-clearing brawl might look chaotic, but it's really a ritual that says a lot about human behaviour

Commentary
Judges and lawyers tell us their favourite Supreme Court rulings involving Beverley McLachlin

Thesis
Schools of identical Prussian carp are here - and they're hungry

Thesis
Intersectionality is a simple concept with deep roots and big implications

Thesis
A traditional approach to caring for Indigenous and trans patients

Environment
Bags, wraps, cups and Styrofoam: here are some steps to curb your single-use waste

Just For Fun
Just remember that, when it comes to claims about health, research is your friend

Energy
Turn your windows into solar panels, plus more ingenuity from U of A spinoff companies

Energy
Solving the challenges behind the system that keeps the lights on

Energy
The properties of this poultry byproduct are handy for purifying water used in industrial processes

Energy
Could an old technology answer some modern problems?

Just for Fun
Too many people think of the technical stuff first. In fact, that's the easy part

Health
Find out where the added sodium, sugar and saturated fats in your foods are coming from

Just For Fun
Need help sorting through the noise? Listen up

Just For Fun
The Edmonton Oilers star skates like the wind and makes it look easy. All we can do is watch in awe.

Did You Know
Journey back in time with one of the internet's most eclectic collections of Prairie documents

Just For Fun
We didn't believe that a paper tube could fly. Turns out, we just had to roll with it

Did You Know
Gather in a circle, hold hands and join in this traditional First Nations celebration of life

Living
Challenge yourself to sit and look at one thing for 10 full minutes

Relationships
Do more than mingle with the potted plants with these 3 tips

Health
Sweets have a bad reputation, according to one expert who debunks the myth in time for holidays

Continuing Education
I thought I was coming to Edmonton for graduate school. It turned into so much more

Thesis
Understanding how you perceive flavour is the first step to expanding your palate
Alumni Awards
David Breakwell, '79 BCom, hockey player and coach

Thesis

Just For Fun
Ah, registration. Get alumni together and eventually the conversation will turn to their experiences signing up for classes. We asked you to share your memories.

Environment
Urban water systems risk running dry. Can research help?

At Home
7 steps to rearrange your pictures, gallery-style

Thesis
If you could download your brain, would you still really be you?

Thesis
Metabolism research could design your optimal diet or give advance warning of disease

Trails
Author Jason Lee Norman transforms a campus memory into a work of flash fiction.

Feature
Artificial intelligence is here to stay. We look behind the hype

Tech
He's not very funny, but he has a lot to tell us
Tech
No. 1: artificial intelligence isn't really artificial

Trails
Illustrations by Rémy Simard

Tech
Two years after the Fort McMurray disaster, there are new tools on the horizon that could better predict a destructive fire

Health
Tips to reframe what it means to be active

Living
Designers share their fashion tips

Profile
UAlberta alumni and students boosted Olympic hopes

Health
4 myths busted by a public health expert

Feature
Cooking, studying, hanging with friends. These mundane activities take on new meaning for three Syrian refugees who are putting their lives back together as U of A students
Feature
There is a magic that happens when you place words alongside a picture. Understanding the interplay can enrich the way we see and think
Alumni Awards
John Hogg, '78 MA, '82 PhD, coach, professor
Alumni Awards
Jane Alexander, '93 MEd, '97 PhD, Bishop of the Anglican Church of Canada
Alumni Awards
Paul Cantor, '62 BA, investment banker, leadership trainer
Alumni Awards
Adam Sweet, '07 BA, '07 BA(SpecCert), Chief of staff, Edmonton Economic Development Corp.

Feature
Three educators discuss how Indigenous and non-Indigenous people can work as allies

Feature
The TRC laid out some difficult truths. Where do we go from here?

Feature
It's so much easier to retreat behind excuses, but healing our relationship with Indigenous peoples first requires self-awareness

Feature
A few facts and findings from the Truth and Reconciliation Commission

Commentary
We ask a journalist, media expert and psychologist for their thoughts on media literacy

Society
New Islamic cultural garden set to open in 2018

Did You Know
Researchers "deactivate" viruses on surgical masks with simple treatment

Health
A special grant lets researchers look at how Alberta wildfires are affecting firefighters' physical and mental health

Did You Know
Something shifted in a big way for Leonard Cohen when he arrived at the University of Alberta in 1966.

Health
A historic gift to the University of Alberta supports research and care for these traditionally underserved populations.
Did You Know
'Verbing' the Future of the U of A

Tech
Discovery
U of A research is always garnering media attention. Here's the lowdown on what's been causing a buzz.

News
Puppy love, mid-life slumps and Zika virus

Living
7 Lessons From a Semester Abroad

Did You Know

News
A brief look at what's new at the U

News
U of A alumni who made headlines recently

News
Respected academic leader and international scholar begins term July 1, 2015
News
A land trust has been approved to provide long-term revenue for the university
News
Catch up on the lastest news about the U of A and alumni

Just For Fun
Hide & Seek Club president Adam Pinkoski shares the "10 commandments of hide-and-seek"
Discovery
The low down on what's up in U of A labs

Did You Know
Figure-skating official finds parallels between sport and leadership

Just For Fun
The U of A has several things worth bragging about. Here is our list of some superlative things on campus

Just For Fun
Spirits to show your school spirit

Society
Glenn Kubish, '87 BA, explains the worth of his education

Health
Meet the people working to make sure your family lives longer — and better

Did You Know
For anyone who ever wondered what their degree was really worth, comes the answer: $12.3 Billion

Profile
Meet one of the U of A's newest students-who just earned more than $100,000 in scholarships

Health
New degree program allows students from across disciplines to embrace a collaborative educational experience

Discovery
Lorne Babiuk receives Gairdner award for leadership in vaccine development and research

Discovery
Investment in research projects aims to improve quantity, quality and sustainability of water in rural Alberta

Relationships
Former Deputy Provost Dru Marshall shares her top 10 tips for building a successful team.
Continuing Education
Two U of A professors follow up on a study that began over two decades ago.

Living

News
U of A business students drive away with top prize at the 2011 Canada's Next Top Ad Executive competition.

Discovery
Electron microscope tip makes Guinness Book of Records.

Feature
A non-grad extends a hand to the U of A in honour of her father.

Health
Prize-winning master's thesis shows promise for prostate cancer

Discovery
U of A research team makes a breakthrough in plastic solar cells

Did You Know
NASA refocuses on a plans for an unmanned mission to mars in 2018.

Discovery
Next time you're stuck on the freeway think of waves radiating outward from a gas explosion.

























































































































































































































































































































































































































































We at New Trail welcome your comments. Robust debate and criticism are encouraged, provided it is respectful. We reserve the right to reject comments, images or links that attack ethnicity, nationality, religion, gender or sexual orientation; that include offensive language, threats, spam; are fraudulent or defamatory; infringe on copyright or trademarks; and that just generally aren’t very nice. Discussion is monitored and violation of these guidelines will result in comments being disabled.