Combining a cancer-targeting virus with radiation to treat brain cancer in mice was more effective than either therapy on its own according to new research, providing hope for new treatments that combine immunotherapy with traditional surgery, chemotherapy or radiation.
The researchers treated mice with glioblastoma tumours simultaneously with high-dose radiation and a genetically engineered vaccinia virus, a virus that has been used safely as a vaccine against smallpox. In humans, glioblastoma is among the deadliest cancers, killing 95 per cent of patients within five years, according to the Brain Tumour Foundation of Canada.
The researchers saw a 15 per cent cure rate among the virus-treated animals and 20 per cent for those that received radiation alone, but 67 per cent of the mice treated with both therapies were cleared of their tumours. The team also re-challenged some of the cured mice with fresh brain cancer cells and found that 62 per cent of the combination-treated mice were able to reject or resist new cancer.
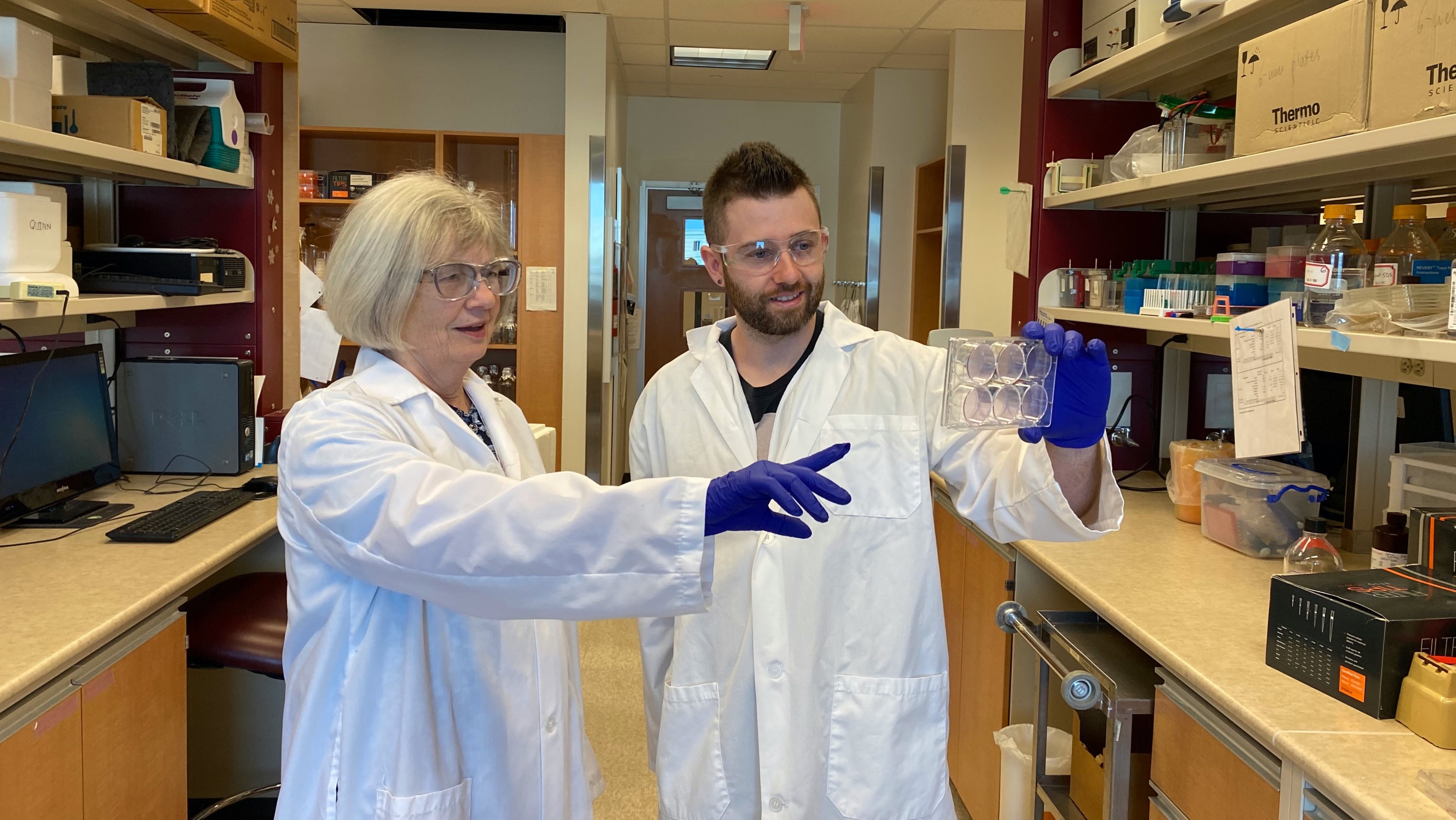
“It was quite remarkable to see that the effect of the combination was greater than either of its parts alone,” says first author Quinn Storozynsky, a graduate research assistant fellow in the Faculty of Medicine & Dentistry who led the research as part of his PhD thesis.
Harnessing viruses to “seek and destroy” cancer cells
Oncolytic viruses work in two ways to fight cancer, Storozynsky explains. First, they are genetically altered to replicate only within cancer cells — literally causing them to explode and spread virus to other nearby cancer cells — while having negligible effects on healthy cells. Second, they counteract the immune suppression caused by tumours, bringing the cancer cells to the attention of the immune system again so it can attack them.
“You need some way to seek and destroy cancer cells, so if you can harness the immune system, that's an incredible way to have this evolutionarily conserved response do the work for you,” he says.
“There aren't many therapies for cancer that work really well on their own because the nature of tumours is that they are not uniform due to high mutation rates, so combinations of therapies have the greatest chance of success,” says principal investigator Mary Hitt, associate professor of oncology.
The team used a strain of vaccinia virus developed by David Evans, professor of medical microbiology and immunology, which Hitt and Evans had previously found effective against bladder cancer. They chose to target glioblastoma because it is very aggressive, with cancerous cells quickly infiltrating other parts of the brain beyond the main tumour site.
“People get surgery,then radiotherapy with chemotherapy at the same time, and then another course of chemo, so it's a very rigorous therapy. But we’ve been using the same approach for more than 15 years, and there's an urgent need for a novel approach to treat glioblastoma,” says Storozynsky.
Using the patient’s own immune system to target cancer
The researchers say their work reinforces the work of others in the relatively new field of immunotherapy, which seeks to use the patient’s own immune system to target cancer.
“Cancer cells are very good at evading the host immune system. They have all these different mechanisms to disguise themselves and avoid being targeted by immune cells. With an oncolytic virus you get this direct killing effect of cancer cells, but then you also alert the immune system that, ‘Hey, look, there's a tumour over here,’ so then you get this antitumour immune response as well,” explains Storozynsky.
He says he would like to see further work done combining vaccinia or other oncolytic viruses with different doses of radiation to learn how to optimize the effect. Hitt suggests testing their combination with another immunotherapeutic agent known as an “immune checkpoint inhibitor,” which interferes with cancer’s anti-immune defence system, to see whether the effectiveness can be amplified even further.
“If you could add that in, then you might get all of the animals protected against new tumours growing,” she suggests.
Although only one oncolytic virus has so far been approved by the U.S. Food and Drug Administration for use in humans and the virus is not yet approved in Canada, Hitt sees more becoming clinically available within the next decade.
“It's a slow process of confirming the safety and effectiveness through clinical trials, but I think it's just a matter of time,” she says.
The research was supported by the Canadian Institutes for Health Research, Alberta Cancer Foundation, Government of Alberta, University of Alberta and the Terry Fox Research Institute. Mary Hitt is a member of the Li Ka Shing Institute of Virology and the Cancer Research Institute of Northern Alberta.