Obstetrics & Gynecology Residency Training Program
Welcome to the Obstetrics & Gynecology Residency Program at the University of Alberta.
Strong
Surgical and obstetrical training with early exposure in a supportive environment.
Unique
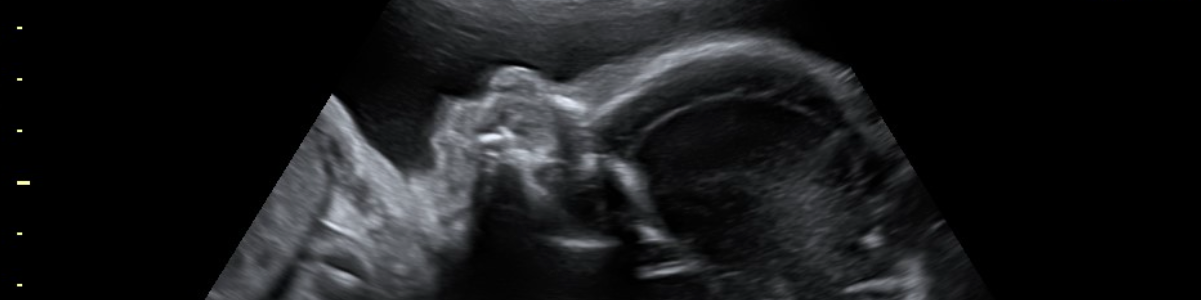
Simulation labs and equipment including ultrasound and laparoscopy.
Diverse
Population of patients: rural, urban, inner city, socially advantaged and disadvantaged women of all ethnicities.
Interview/CaRMS Specific Information
Our interviews will be online in the format of a MMI.
The candidates will rotate through 6 stations (one station is a one on one with the PD or assistant PD) using zoom. Through our interview process we aim to select candidates that demonstrate compassion, excellent communication skills, collaboration, motivation for lifelong learning and empathy.
Canadian applicants to our Residency Training Program in Obstetrics and Gynecology must apply through the Canadian Resident Matching Service (CaRMS). Please consult the CaRMS website open in a new tab for guidelines and requirements.
For general questions or admission inquiries, please contact the Residency Program Administrator.
Our Indigenous Admissions Pathway selects qualified, self identified Indigenous applicants through a separate subcommittee that consists of Elders (voting) and faculty (non-voting). Anyone wishing to enter this pathway should identify themselves to the Program Administration obgynpme@ualberta.ca
Contact Us
Dr. Christa Aubrey
Residency Program Director
Obstetrics & Gynecology
Email: preuss@ualberta.ca
Dr. Valerie Capstick
Assistant Program Director
Obstetrics & Gynecology
Email: capstick@ualberta.ca
Sarah Skelton & Lalitha Srinivasan
Program Administrators
Email: obgynpme@ualberta.ca
Address:
Obstetrics & Gynecology
Room 5S 131 Lois Hole Hospital., Robbins Pavilion RAH
10240 Kingsway Avenue
Edmonton, Alberta, T5H 3V9
Welcome to the Obstetrics & Gynecology Residency Program at the University of Alberta (U of A)

Dr. Christa Aubrey
Residency Program Director
I am excited to take on this role. I completed my medical school and Residency in OBGYN at the University of Alberta, along with the Clinician Investigator Program (CIP), and subsequently a fellowship in Gynecologic Oncology at the University of Calgary. I have spent the past year under the direction of our previous Program Director, Dr. Capstick, and along with a couple of our residents, exploring our "hidden curriculum". We are committed to improve not only the excellent surgical, obstetrical, and clinical experience but also the culture of the residency program. I am looking forward to working with our dedicated group of residents and faculty over the upcoming years!

Dr. Val Capstick
Assistant Residency Program Director
I am proud to announce that our program has survived the challenges of COVID and accreditation thanks to the amazing residents and dedicated faculty who make up our Department.
We train exceptional generalist Obstetrician Gynecologists as well as future Subspecialists. Our program has very strong surgical training as well as excellent obstetric experience. Research is encouraged and expected. Our seniors preparation for the Royal College exams is a group effort, with numerous faculty offering practice exams and review sessions.
The challenges of the previous few years have created an amazing cohesive team from the residents to the Residency training committee to our department administration.
Our Program
Our program trains strong generalist OBGYNs and is an excellent preparation for entry into subspecialty training. Our program has been successful thanks to our resilient program and supportive faculty.

Large volume of patients from diverse backgrounds.



Residents have travelled nationally and internationally, most recently Africa, and Australia.

The ratio of faculty to residents is five to one. We have perinatologists, gynecologic oncologists, reproductive endocrinologists, urogynecologists, and many generalists.

There are 6 funded positions per year.
Overview Video
The Obstetrics and Gynecology Residency program at the University of Alberta is made up of a friendly, supportive, and collegial group of residents and features unique learning resources and rotations. The city of Edmonton provides an environment where residents can achieve work-life balance to suit a wide array of interests.
Residency at a Glance
UAlberta's Obstetrics and Gynecology Residency Training Program is centered at the Royal Alexandra Hospital (RAH) in Edmonton. The RAH is the tertiary Obstetrics and Gynecology referral centre for northern Alberta, parts of northern British Columbia and parts of the Northwest Territories. RAH houses the Lois Hole Hospital for Women (LHHW), a leading centre in Women's Health, which receives approximately 75,000 patient visits annually. Our residents also spend time at three community hospitals in the Edmonton area: the Grey Nuns Hospital, the Misericordia and the Sturgeon General.
There are 6 funded residency positions per year and approximately 30 residents in the program. Residents work with a supportive and dynamic team of educators, clinicians and researchers throughout their training. Current academic faculty includes 8 perinatologists, 6 gynecologic oncologists, 7 reproductive endocrinologists, 5 urogynecologists, 1 urogynecologic fellow, 7 basic scientists and approximately 100 generalist OBGYNs.
Our residency program was reviewed in October 2020 and received full accreditation from the Royal College of Physicians and Surgeons of Canada. Our graduates consistently excel in the national Royal College examinations and go on to enjoy rewarding careers in gynecological and obstetrical medicine across Canada and beyond.
The RPC (Residency Program Committee) reviewed our curriculum as CBD was initiated and made some changes for the 2021 year. This is the most significant change in the last few decades. The focus has been creating more flexibility in training. We moved all of our subspecialty rotations to third year and reduced them to 2 blocks. Gyne Oncology and MFM are revisited in fourth year.
In the first year, resident training is focused on Core Surgical Training. We have been part of the RCPSC Surgical Foundations program for over 15 years, and our residents have taken the Surgical Foundations RCPSC exam for the past 5 years. It has become a mandatory part of Obstetrics and Gynecology RCPSC training commencing in 2016.
PGY-1 training includes:
- 2 blocks of Transition to Discipline (TTD) at start of residency
- 2 blocks of General Surgery
- 2 blocks of Internal Medicine
- 1 blocks of Emergency Medicine
- 1 block of Obstetric Ultrasound
- 1 block of NICU/Ob Anaesthesia
- 3 blocks of general obstetrics and gynecology
- 1 block of vacation
Residents attend the Surgical Foundations half days on Wednesday mornings. There may be opportunities to attend the OBGYN half day on Wednesday afternoons. It is expected that the resident will complete the Surgical Foundations Program by the end of the first year.
Program of Assessment: PGY-1
- Entrustable Professional Activities (EPA) Assessments & Procedure Logs
- Intraining Evaluation reports (ITERS)
- Surgical Foundations Assessments
- MCC Exam (part two)
- Minimally Invasive Surgery Wet Labs (Surgical Foundations)
- Dry Labs
- Ultrasound Rotation Exam
During the second year, our residency program focuses on the management of high-risk Obstetrics and General Gynecology basic surgical skills. Training includes 10 months of Core Ob/Gyn studies carried out at the Royal Alexandra Hospital and the Grey Nuns Hospital sites. It is expected that the resident will be close to completing the Foundations of Discipline Stage (OBGYNE) by the end of the PGY 2 and starting on some CORE EPAs.
We also provide exposure to a block at the Women's Health Options, (family planning) and 2 blocks in ICU.
Program of Assessment: PGY-2
- Entrustable Professional Activities (EPA) Assessments & Procedure Logs
- In-Training Evaluation Reports (ITERs) Assessments
- Half Day Presentations (evaluations are conducted by fellow residents)
- Canadian National MCQ Exam (previously known as APOG exam)
- Bi-Annual Objective Structured Clinical Examination (OSCE)
- Minimally Invasive Surgery Wet Labs
- Surgical Foundations Exam
- The Council on Resident Education in Obstetrics and Gynecology (CREOG) Exam (optional)
- CanMeds OSCE Exam (within Surgical Foundations Program)
- EPA OSCE Exam (OBGYN) 2x a year
The third and fourth years of our program focus on subspecialty training, including:
- 3 blocks of Maternal-Fetal Medicine (MFM), one of which is OB medicine
- 2 blocks of Reproductive Endocrinology & Infertility (REI)
- 3 blocks of Gynecologic Oncology (GYN ONC)
- 2 blocks of Urogynecology (UROGYN)
- 4 blocks of Chief resident rotations in 4th year
- 1 block of Minimally Invasive Surgery rotation
- Approximately 5 blocks of selective/elective (3 blocks of elective of the residents choice, pending approval by the program director).
- 2-4 blocks of Community OBGYN (GNH and other)
Program of Assessment: PGY-3/4
- Entrustable Professional Activities (EPA) Assessments & Procedure Logs
- In-Training Evaluation Reports (ITERs) Assessments
- Ultrasound Exam - Maternal Fetal Medicine (MFM)
- Written Rotation Exam (MFM rotation)
- Oral Exam - Reproductive Endocrinology and Infertility Rotation
- Canadian National MCQ Exam (previously known as APOG)
- Minimally Invasive Surgery Wet Labs
- Bi-Annual Objective Structured Clinical Examination (OSCE)
- The Council on Resident Education in Obstetrics and Gynecology (CREOG) Exam (optional)
- Grand Rounds Subspecialty Presentations
- Fundamentals of Laparoscopic Surgery Exam (in progress)
In the final year of residency, students grow in their roles as Chiefs acting as Junior Consultants in Labor and Delivery, and prepare for their Royal College Examinations. The PGY-5 year is divided as follows:
- Variable number of blocks as Chief or senior resident (RAH, GNH, MCH & SCH)
- 4 blocks of ambulatory care (currently before spring RC exams. When CBD residents are in R5, 2 blocks will move to the fall prior to the written exam)
- elective/selectives
Program of Assessment: PGY-5
- Entrustable Professional Activities (EPA) Assessments & Procedure Logs
- In-Training Evaluation Reports (ITERs) Assessments
- National Review Course (Objective Structured Clinical Examination (OSCE) and written exam)
- Minimally Invasive Surgery Wet Labs
- Chief OSCE Exam
- Journal Club Presentations
- Self Reflective Evaluations
- Centre for the Advancement of Minimally Invasive Surgery (CAMIS) Sessions
- Grand Rounds Presentations
Teaching Sites
The residency program is based at the Lois Hole Hospital for Woman, at the Royal Alexandra Hospital open in a new tab. This is the tertiary referral center for Northern Alberta, parts of northern British Columbia and parts of the NWT and Nunavut. The University Department of Obstetrics and Gynecology is based at the RAH. The majority of academic medical departments are based at the University of Alberta Hospital.
Three community hospitals have residents continuously, the Grey Nuns Community Hospital open in a new tab, Misericordia Community Hospital open in a new tab and Sturgeon Community Hospital are full service hospitals with busy Obstetrical and Gynecologic Surgery services. The Gynecologic Oncologists operate at the Lois Hole Hospital and see outpatients at the Cross-Cancer Institute.
Program Supports
- Mentor Groups’ with residents from R1 to R5 for support from your colleagues. Our residents created these groups on their own initiative.
- ‘Buddy call’ system for introduction to Obstetrical call
- Large number of faculty with direct responsibilities in the residency program
- Committed Academic Advisors for each resident
- Advocacy and Wellness Office in PGME, as well as PARA
- Residency wellness subcommittee of RPC
- Resident membership in Academic Half Day, Curriculum Innovation and CaRMs subcommittees
Subspecialties
Subspecialties of Obstetrics and Gynecology include:
- MFM (Maternal Fetal Medicine)
- REI (Reproductive endocrinology and infertility)
- UROGYN (Urogynecology)
- GYN ONC (Gynecologic Oncology)
- Special interest areas include: Family planning, sexual dysfunction, STIs, Mature Women’s Health, Pelvic Pain, Advanced Minimally Invasive surgery
Currently, we offer a urogynecology fellowship program.







