Dr. Bo (Cloud) Cao to Head New Study on Impact of Cannabis-Based Medications on Opioid Use Outcomes
Gary Lamphier - 25 May 2021
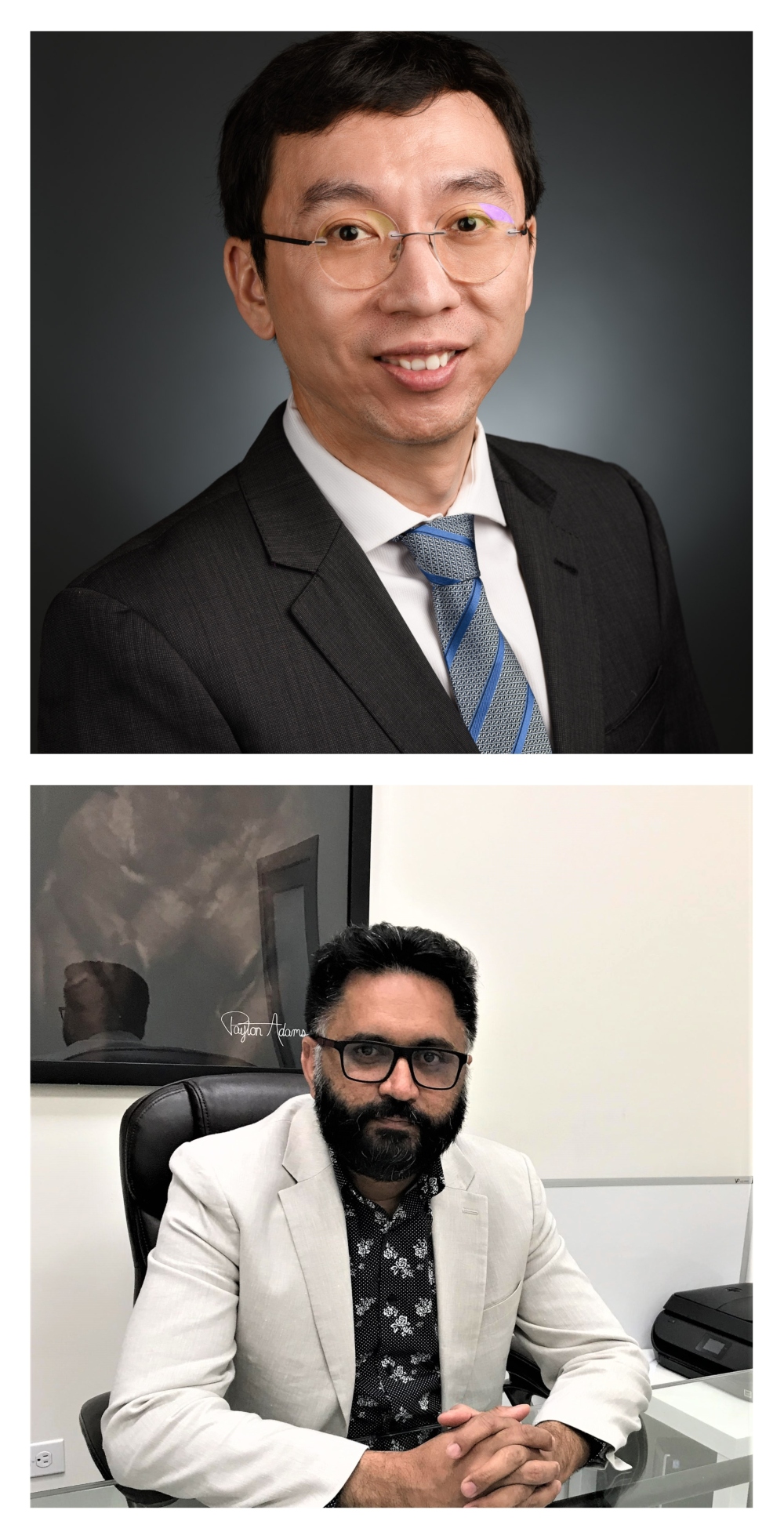
Top: Dr. Bo Cao Bottom: Dr. Avininder Aulakh
The $299,717 study is one of three research projects funded under Alberta Innovates’ mCannabis.Real World Program, which seeks to address what it calls “urgent clinical or policy knowledge gaps” regarding the efficacy and safety of cannabis use among patients in the broader community.
Dr. Cheryl Sadowski, a Professor in the Faculty of Pharmacy and Pharmaceutical Sciences, is leading a separate $300,000 study on cannabis use in rheumatology patients.
Dr. Suzette Brémault-Phillips, an Associate Professor in the Faculty of Rehabilitation – Occupational Therapy, is heading a third study, focused on understanding the medical value and risks for veterans of medicinal and recreational cannabis use. It also received $300,000 in funding.
The total value of the three studies is $930,000, with Alberta Innovates contributing 97% of the funding. All three studies are scheduled to run from March 2021 to March 2023.
“Real-world data are sources of information collected outside of conventional randomized clinical trials. This type of information can provide evidence about the health outcomes of diverse patient populations in a real-world setting and provide important economic insights to inform clinical or policy decisions,” Alberta Innovates said, in announcing the awards.
Dr. Cao’s research will be based on anonymized administrative data from Alberta Health and Alberta Health Services. It will also incorporate feedback from patient and stakeholder focus groups to gain a deeper understanding of the overall context and related issues around the use of prescription opioids and medical cannabis.
“We are focusing on a specific population of patients who use both prescription opioids and prescription cannabis, specifically the synthetic cannabis (Nabilone) that is usually used by cancer patients to avoid vomiting and nausea, but it’s also used by other patients. We’re not looking at street drugs,” explains Dr. Cao.
“We don’t have good data for the street market or recreational cannabis, but that’s our longer-term goal. The bigger picture is, we want to know how cannabis use affects opioid outcomes.”
Dr. Cao says he hopes his findings will shed some light on whether cannabis reduces or increases the risk of developing Opioid Use Disorder (OUD) or overdose.
“There is a big debate about whether cannabis – in particular, medical cannabis – reduces or increases the risks associated with drugs like opioids. We don’t yet know the answer. In the scientific literature there is a well-known study showing that introducing cannabis may lower opioid dosage and subsequent risk for OUD or overdose in the short term,” he notes.
“But another populational study with a longer period of follow-ups found that cannabis increased the risks of people developing OUD. So there is a huge debate about this, and one of the objectives of the mCannabis RealWorld Program is to identify the benefits and the risks of cannabis-based medicine.”
Dr. Cao hopes to eventually expand the scope of his research to include other cannabis-based medications, as additional data becomes available, to determine what if any impact it has on opioid related outcomes.
“Part of the debate around cannabis is, will cannabis serve as a gateway drug that leads to other addictive drugs for some populations, even though cannabis itself is safe to use? Or do the medical benefits outweigh any potential risks? We just don’t know. I think this whole field needs a lot more research, so that’s why we’re doing this type of study, thanks to the support of Alberta Innovates.”
One experienced addictions treatment specialist who sees a connection for some individuals between recreational cannabis use and subsequent risk of addiction to street drugs like cocaine, fentanyl and heroin is Dr. Avininder (Avi) Aulakh.
Dr. Aulakh, formerly the Clinical Lead for Alberta Health Services’ Opioid Dependency Program in Edmonton, operates the Savera Medical Centre in southeast Edmonton, which is dedicated to treating opioid, alcohol and/or other substance use addictions.
“When we look at the patients we see here, rarely do they have struggles with only one substance. There is often a crossover. If they are addicted to one substance, they are also at risk of being addicted to something else,” says Dr. Aulakh, who is also a Clinical Lecturer in the Department of Psychiatry.
“But it’s fair to say that based on our clinical interactions with patients, most of them started with cannabis. That is often the first illicit substance they tried, apart from drinking or smoking, when they were say 14 or 15 years of age, and they moved on from there to other substances including opioids,” he explains.
“That said, we’re dealing with the subset of the population that is struggling with addiction. Many people may try cannabis and don’t have any struggles with it. But cannabis is a gateway to other drugs for some people, and once opioids come into play, that becomes the dominant drug. The earlier cannabis use starts, the more likely a person is to develop addictions. If someone started using cannabis at 14 versus 18, with all the same risk factors, at 14 the risks (for addiction) are much higher.”
Prescription opioids are mainly used to treat acute and chronic pain. But they are also used to control persistent cough or diarrhea, or to treat opioid addiction with methadone or buprenorphine-naloxone, under the supervision of a healthcare professional.
According to a 2017 report by the Canadian Centre on Substance Use and Addiction, prescription opioids were used by 13% of the Canadian population (roughly 4.75 million people) to relieve pain. Among those using opioid pain relievers, 2.2% or more than 80,000 Canadians reported using them for non-medical purposes, the report said.
“For the pilot study we’re doing, if you look over the past five years in Alberta there were about 1.2 million people in total who used opioids, so it’s a large number. But it’s a much smaller number of people who used both prescription opioids and medical cannabis, says Dr. Cao.
“The latter group may involve up to 10,000 people, but this group may help us to understand their prescription opioid related outcomes. This is a starting point for us to understand general cannabis-based medicine and its interaction with prescription and non-prescription opioids,” he adds.
“In our study, the Computational Psychiatry Group will be utilizing Machine Learning to help us make individualized predictions about future risk levels relevant to opioid outcomes. For some people, medical cannabis could present a higher risk for opioid addiction down the road, but for others it may present a lower risk.”
Since data analysis alone won’t provide a comprehensive picture of all the factors that lead to OUD and opioid overdose, Dr. Cao stresses that input from clinicians and opioid and cannabis users who draw on their owned lived experience will be an important part of the study. Alberta Innovates and Alberta SPOR SUPPORT Unit (AbSPORU) helped to engage people with lived experience since the early stage of the study.
“That’s the beauty of the real-world component, and why we need to include focus groups to identify factors we don’t see from the data. People who have lived experience can tell us what we’re missing, so that’s why we need to be super-cautious about making any generalizations,” he says.
“There will be things we didn’t consider or we won’t see from the data. But we want to know what they are, so we’ll know what the study limitations are, and to what extent we can use this type of tool to help clinicians, patients and stakeholders in future.”