Judgment-free “conversation clinic” offers vaccination advice for expecting parents
Kirsten Bauer - 17 December 2021
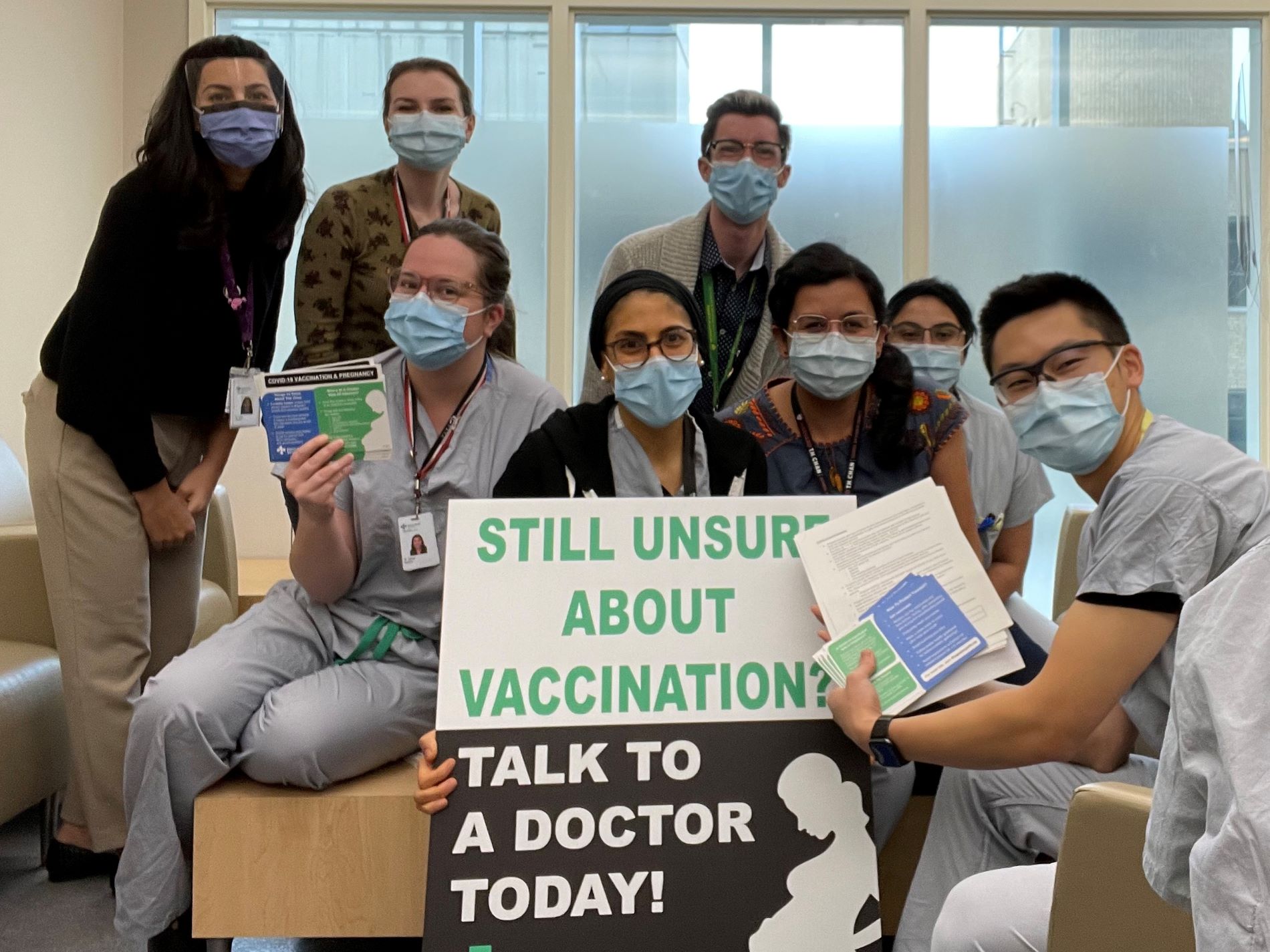
Obstetrics and gynecology residents raised awareness about COVID-19 vaccines and pregnancy on their October 6th day of action.
Each year, obstetrics and gynecology resident physicians at the University of Alberta hold a day of advocacy to work on projects relating to improving public health and safety. Residents typically focus on cervical cancer, but the COVID-19 pandemic sparked a new idea this year: to help those who are pregnant feel confident about getting vaccinated by offering judgment-free zones, where expecting parents could safely ask questions without feeling pressure to make a decision.
“From July through October this year, we'd seen the highest number of pregnant patients in the ICU that we had ever seen,” said Laura Sevick, a second-year resident in the program. “It was reaching a point where we were trying to create new strategies for things that we just haven't ever had to think about in our specialty. Usually we have one patient, if any, in the ICU.”
“We've had a number of patients who ended up in ICU, were intubated due to COVID-19, and needed emergency caesarean sections while intubated,” added Sarah Shamiya, a third-year resident in the program. “We even had a case where a patient passed away after delivering her baby while intubated, and I think all of that precipitated the idea for the topic.”
In the Q&A below, Sevick and Shamiya explain how their experience of learning through the COVID-19 pandemic inspired the October 6th day of action.
How did you get the idea for a conversation clinic?
Sevick: When we originally started, my hope was to have a whole vaccination clinic, but it quickly became clear that a lot of people within our department had similar ideas and had already laid quite a bit of the groundwork. They were able to share with me the logistical roadblocks that they faced in terms of organizing a full clinic, including vaccine supply and logistical challenges. So we started thinking, “If it can't be a vaccination clinic, what are some other things we could do?”
People are ultimately trying to do what is best for their baby, so we decided to create a space where a pregnant person could ask any question, and it wouldn't be met with judgment or pushback. That eventually led to creating the judgment-free zones outside the maternal fetal medicine clinic at the Lois Hole Hospital for Women, as well as at Kingsway Mall.
Shamiya: It sounds like it's a project that took time to evolve, but this literally happened over the course of two to three days. I think the positive feedback and support from our staff really motivated us and it trickled down to the rest of our residency group.
Sue Chandra (maternal fetal medicine specialist, Department of Obstetrics & Gynecology) originally suggested a “non-judgment zone” where someone could come and just ask their questions about a vaccine. May Sanaee (urogynecologist, Department of Obstetrics & Gynecology) was also really passionate about this project, and largely organized our time at Kingsway Mall, and her partner created brochures and posters.
Another group that got involved was Action For Healthy Communities (AHC), a non-profit organization. For those people who decided they wanted to get the vaccine, they worked with the pharmacy in the mall to arrange walk-ins, and they were happy to help.
What are some common concerns people expressed about vaccination?
Sevick: The primary concern was that this vaccine was created too rapidly, and the original trials did not include pregnant women. A lot of the people that we talked to were hesitant in the context of being pregnant, so we heard many say, “As soon as the baby's born, I'll get vaccinated.”
When we hear people say things like that, we tell them, “I think we understand where you're coming from. We hear your concerns, but what I know to absolutely be true is that if you were to get COVID-19, we see risks like placental insufficiency or a greater risk of needing intubation, or ICU care.” And we have now seen maternal deaths from this, so I think for a lot of people, it's helpful for us to just be able to say vaccination during pregnancy is safe and I would recommend it in all instances.
Shamiya: What most pregnant patients want is the safety of their baby. I've noticed a lot of vaccine promotion focuses on patients, and our patients would give up anything for their baby, so they don't care if they’re sick so long as baby's OK. We help them to recognize that their well-being really dictates the well-being of their baby as well.
Our ultimate goal is the same. We want a healthy baby and a healthy mom. Sometimes having that discussion with patients helps remove the barrier a bit more.
How has this pandemic experience affected you?
Shamiya: In all honesty it has been really, really, really difficult. I think any surgical residency is really hard, but COVID-19 has hindered a lot of our training. For the majority of my urogynecology rotation, for example, I had limited OR exposure because they were limited to emergent surgeries only. Even cancer surgeries had to be delayed.
When you're constantly in survival mode, human beings in general have only so much capacity. When it's more than 19 months, and you're already working in an emotionally charged environment, the burden of the pandemic can expedite burnout, which we know is endemic in physicians and other health-care workers. We're lucky that our program is cognizant of this and is supportive, but it still does impact us.
Sevick: I entered residency in the pandemic, so I have only ever practised medicine inside of the COVID-19 pandemic. A lot of the celebrations and excitement that come with completing medical school and starting residency have all been taken away. I never graduated. I've never been to a Journal Club in person. I've never been to a Grand Rounds in person. I've never been to an academic half-day in person. Most of the staff have never seen my face in its entirety, so I think that's come with a huge emotional toll.
We enter ICU rotations in our second year, so I'm there right now. Just in the last two months we’ve seen the highest volume of ICU admissions that we've ever seen in Edmonton. We've had to adapt to constantly changing schedules and expectations.
It's been a strange time to learn how to practise medicine. But I think we've all learned that we're probably way more resilient than we ever thought we were. Even in times when you feel really isolated and you're being told to isolate, you're not alone. I've never felt alone in this whole process. Some really amazing relationships have developed despite everything.